Retinal Detachment in a Nut Shell
Dr. Stephanie Joan Mak, B.Sc., O.D.
Doctor of Optometry Graduate, University of Waterloo, Canada
Keywords: optometry, retinal detachment, vision loss
Inside our eyes, there is a transparent jelly called the “vitreous humour” and a tissue layer at the back called the “retina”[1]. The retina acts like a screen: it absorbs light entering the eye, then relays the light information to the brain, allowing us to see the world[1]. That is how we can see the world around us. As we grow older, proteins in the vitreous humour will lose its transparency and begin to clump up into solid flakes or strands that float around in the eye[3]. The shadows formed by these flakes or strands are what we call “floaters”[3]. Some people start noticing floaters in their 20s; this is completely normal.
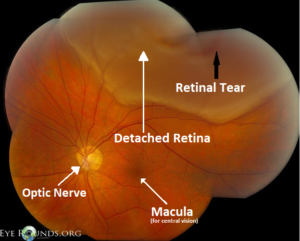
Figure 1. Photograph of the eye interior depicting a detached retina and retinal tear[8].
As we age, the vitreous humour will liquefy and shrink, which pulls the vitreous humour off the retina[1,3]. This is called a “posterior vitreous detachment (PVD)”, and is harmless in most cases. In rare cases, the vitreous humour may tear a hole in the retina as it is separating from it[1,3]. Fluids could enter underneath that hole/tear and lift off the whole retina, causing a “retinal detachment”[1,3]. Retinal detachments can occur in people of all ages, but are most common in those over 40 years old[1,2].
Retinal detachment is a medical emergency; if the retina is not re-attached within 1-2 days, permanent vision loss could result. The symptoms of retinal detachment can be summarized into 4 F’s: 1)Floaters (a sudden, severe increase in floaters) 2) Flashes (a camera flash-like sensation in your vision), 3) Falling Curtain (a black curtain falling in any direction, up, down, left, or right) , and 4) Failing Vision [3,4,8]. If you experience any of the above symptoms, you must see an optometrist immediately; this is a medical emergency that requires urgent treatment. The optometrist will dilate your pupils to examine the back of the eyes. If a retinal detachment or tear has occurred, a urgent referral will be made to an ophthalmologist for surgical treatment[4]. It is possible to recover most of your vision if the retinal detachment is treated promptly[4]. Delayed treatment, however, could result in permanent vision loss[4].
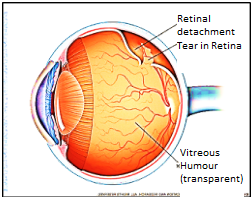
Figure 2. A retinal tear which resulted in a retinal detachment[9].
Who is at risk of retinal detachment? People who have severe near-sightedness (greater than -6 diopters) have a higher risk of retinal detachment[1,4,6]. The more severe the near-sightedness, the longer the eyeball becomes. This stretches retina thin[4,5]. At some point, the retina will no longer be able to withstand the tension and a hole/ tear forms, which could result in a retinal detachment[4]. Other risk factors of retinal detachment include: eye inflammation, eye surgery (e.g. cataract removal), diabetic eye disease (proliferative diabetic retinopathy), eye injuries, lattice degeneration (thinning of the peripheral retina), pilocarpine eye drops, family history of retinal detachment, and/or previous history of retinal detachment[1]. For people who have had cataract surgery, the increased risk of retinal detachment can last for up to 20 years after surgery[7].
References
[1] Dahl, A. A. & Stöppler, M.C. (2017, October 13). Retinal Detachment. Retrieved from https://www.medicinenet.com/retinal_detachment/article.htm
[2] National Eye Institute. (2009, October). Facts About Retinal Detachment. Retrieved from https://nei.nih.gov/health/retinaldetach/retinaldetach
[3] WebMD. (2017). Eye Floaters: Causes, Symptoms, and Treatment. Retrieved from https://www.webmd.com/eye-health/benign-eye-floaters#1
[4] Lai, T.Y.Y. (2007, September). Retinal Complications of High Myopia. The Hong Kong Medical Diary. 12(9), 18-20. Retrieved from http://www.fmshk.org/database/articles/07mb05.pdf
[5] Curtin, B. J., & Karlin, D. B. (1970). Axial length measurements and fundus changes of the myopic eye. I. The posterior fundus. Transactions of the American Ophthalmological Society, 68, 312–334. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1310382/
[6] The Eye Disease Case-Control Study Group. (1993, April 1). Risk Factors for Idiopathic Rhegmatogenous Retinal Detachment, American Journal of Epidemiology,137(7), 749–757, https://doi.org/10.1093/oxfordjournals.aje.a116735
[7] Erie, J. C., Raecker, M. E., Baratz, K. H., Schleck, C. D., & Robertson, D. M. (2006, December). Risk of retinal detachment after cataract extraction, 1980-2004: a population-based study. Transactions of the American Ophthalmological Society, 104, 167–175. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1809901/
[8] Montague, C & Vislisel, J. (2016). This photograph shows a superior rhegmatogenous retinal detachment that is not yet involving the macula [Fundus Photograph, Labels Added]. Retrieved from https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/Rhegmatogenous-ret-detach.htm
[9] Mayo Foundation for Medical Education and Research. (2017). Retinal Detachment [Multimedia image, edited]. Retrieved from https://www.mayoclinic.org/diseases-conditions/retinal-detachment/multimedia/retinal-detachment/img-20006758.
Post Reviews:
No reviews yet...